Primary care/population health and health economics
Work package six
Researchers in the Primary care, population health and health economics component are developing and validating risk prediction models to identify patients at the highest risk from the UK primary care settings, who are most likely to benefit from the targeted lung health checks (TLHC) and/or low-dose computerised tomography (LDCT) screening, and evaluate the cost-effectiveness (value for money) of the lung cancer screening models for the NHS.
The primary care component project aims to identify potential opportunities for improved diagnostic and cost-effectiveness for lung cancer screening in the UK population.
Download the protocol for QResearch (Primary care) contribution to this work package, including details of how to cite it, here.
For more information about the role of QResearch, see here.
The statistical and health economic models can be used to predict the likely impact of using different thresholds of lung cancer risk for low-dose computerised tomography (LDCT) at the population level, measure and assess the effects of cancer risk across a number of timeframes (short-term, medium-term, and long-term effects, e.g. 1-year, 5-year, 10-year risk of developing lung cancer), and identify ineffective strategies so that they can be refined or avoided.
As primary care is the foundation of the UK health system, one research objective is to characterise the current primary care pathways of lung cancer – from patients present symptoms to their GP, the GP sees them, orders tests, refers them to hospital, to a diagnosis of cancer is made. We are also looking at the treatment which patients received and the length of survival after the diagnosis of cancer. Please see the diagrams in Figures 1 and 2 which illustrate this research process. We will analyse linked anonymised electronic health records from the QResearch database. This will provide research evidence of the current diagnostic pathways. We plan to conduct a similar study after the TLHC and/or LDCT is implemented national wide. This information will help us evaluate the extent to which the TLHC and/or LDCT changes the diagnostic pathways of lung cancer and improve clinical outcomes for patients – for example, whether more patients are diagnosed through screening, whether diagnoses are made at an earlier stage, and whether this is associated with better survival outcomes.
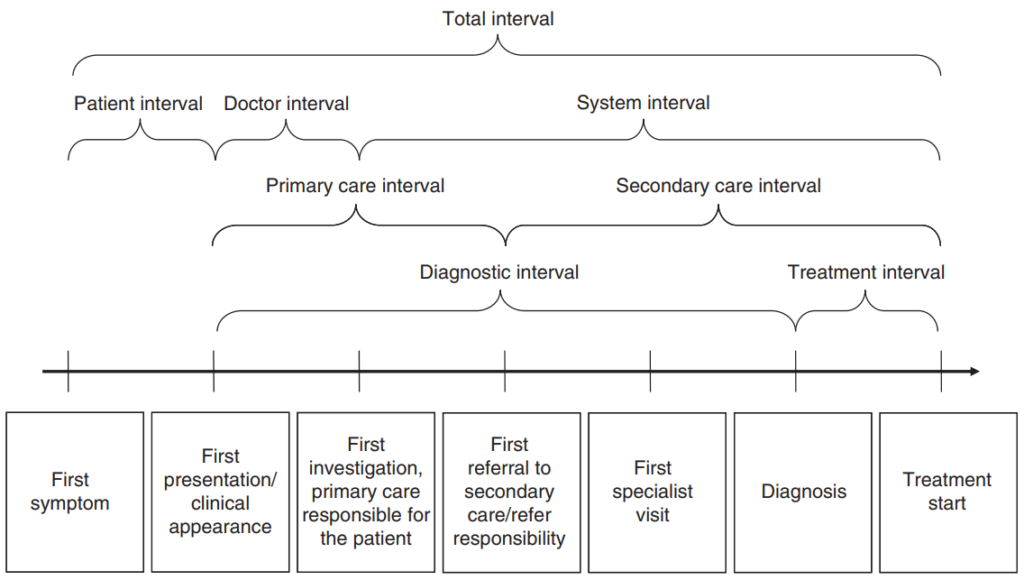
Figure 1 – An illustration of the milestone events and different intervals in the cancer care pathways from the first symptom to the start of treatment (Olesen et al., 2009)
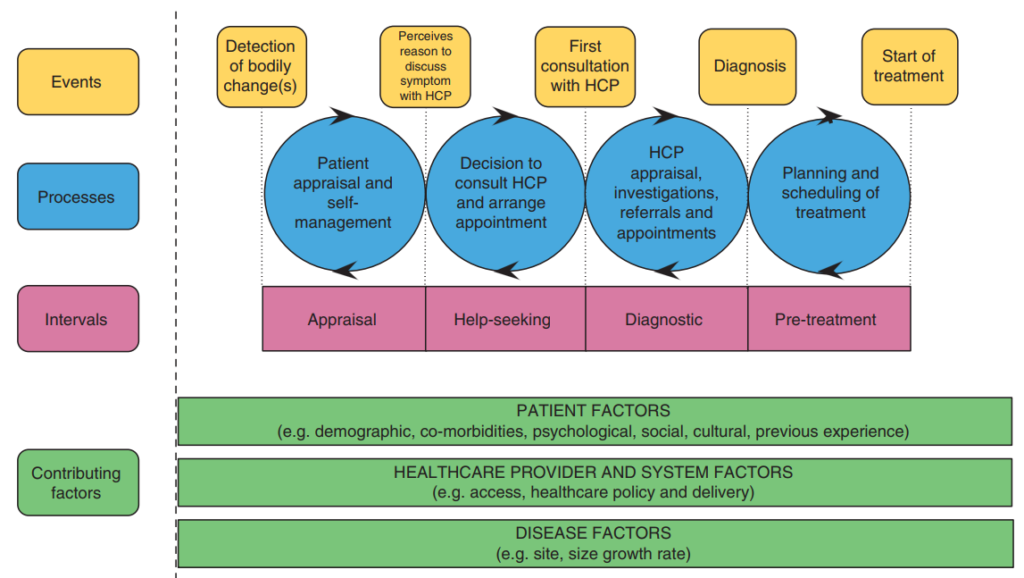
Figure 2 – A conceptual model of cancer pathways to treatment (Walter et al., 2012)
References
OLESEN, F., HANSEN, R. P. & VEDSTED, P. 2009. Delay in diagnosis: the experience in Denmark. Br J Cancer, 101 Suppl 2, S5-8.
WALTER, F., WEBSTER, A., SCOTT, S. & EMERY, J. 2012. The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy, 17, 110-8.
Work package 6 (primary care/population health and health economics) is led by Prof Julia Hippisley-Cox and Prof Sarah Wordsworth, supported by Dr James Buchanan, Dr Weiqi Liao, Dr Liz Stokes and Dr Allison Hirst.
Researchers who work on this package
No related organisations found





